Westerlund E, Jerene D, Mulissa Z, Hallström I and Lindtjørn B. Pre-ART retention in care and prevalence of tuberculosis among HIV-infected children at a district hospital in southern Ethiopia. BMC Pediatrics 2014, 14:250
Abstract
Background The Ethiopian epidemic is currently on the wane. However, the situation for infected children is in some ways lagging behind due to low treatment coverage and deficient prevention of mother-to-child transmission. Too few studies have examined HIV infected children presenting to care in low-income countries in general. Considering the presence of local variations in the nature of the epidemic a study in Ethiopia could be of special value for the continuing fight against HIV. The aim of this study is to describe the main characteristics of children with HIV presenting to care at a district hospital in a resource-limited area in southern Ethiopia. The aim was also to analyse factors affecting pre-ART loss to follow-up, time to ART-initiation and disease stage upon presentation.
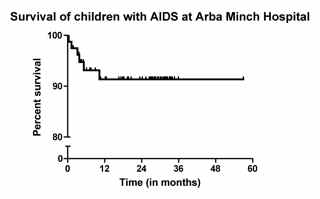
Methods This was a prospective cohort study. The data analysed were collected in 2009 for the period January 2003 through December 2008 at Arba Minch Hospital and additional data on the ART-need in the region were obtained from official reports.
Results The pre-ART loss to follow-up rate was 29.7%. Older children (10-14 years) presented in a later stage of their disease than younger children (76.9% vs. 45.0% in 0-4 year olds, chi-square test, chi2 = 8.8, P = 0.01). Older girls presented later than boys (100.0% vs. 57.1%, Fisher’s exact test, P = 0.02). Children aged 0-4 years were more likely to be lost to follow-up (40.0 vs. 21.8%, chi-square test, chi2 = 5.4, P = 0.02) and had a longer time to initiate ART (Cox regression analysis, HR: 0.50, 95% CI: 0.25-0.97, P = 0.04, controlling for sex, place of residence, enrolment phase and WHO clinical stage upon presentation). Neither sex was overrepresented in the sample. Tuberculosis prevalence upon presentation and previous history of tubercolosis were 14.5% and 8% respectively.
Conclusions The loss to follow-up is alarmingly high and children present too late. Further research is needed to explore specific causes and possible solutions.

 This difference persists also when controlling for age, clinical stage and number of CD4 cells at treatment start Both men and women received the same treatment. Does anyone know about similar trends from other countries?
This difference persists also when controlling for age, clinical stage and number of CD4 cells at treatment start Both men and women received the same treatment. Does anyone know about similar trends from other countries?