 Dangisso MH, Datiko DG, Lindtjørn B (2014) Trends of Tuberculosis Case Notification and Treatment Outcomes in the Sidama Zone, Southern Ethiopia: Ten-Year Retrospective Trend Analysis in Urban-Rural Settings. PLoS ONE 9(12): e114225. doi:10.1371/journal.pone.0114225
Dangisso MH, Datiko DG, Lindtjørn B (2014) Trends of Tuberculosis Case Notification and Treatment Outcomes in the Sidama Zone, Southern Ethiopia: Ten-Year Retrospective Trend Analysis in Urban-Rural Settings. PLoS ONE 9(12): e114225. doi:10.1371/journal.pone.0114225
Background: Ethiopia is one of the high tuberculosis (TB) burden countries. An analysis of trends and differentials in case notifications and treatment outcomes of TB may help improve our understanding of the performance of TB control services. Methods: A retrospective trend analysis of TB cases was conducted in the Sidama Zone in southern Ethiopia. We registered all TB cases diagnosed and treated during 2003–2012 from all health facilities in the Sidama Zone, and analysed trends of TB case notification rates and treatment outcomes.
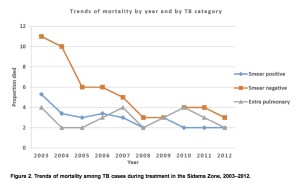
Results: The smear positive (PTB+) case notification rate (CNR) increased from 55 (95% CI 52.5–58.4) to 111 (95% CI 107.4–114.4) per 105 people. The CNRs of PTB+ in people older than 45 years increased by fourfold, while the mortality of cases during treatment declined from 11% to 3% for smear negative (PTB-) (X2 , trend P,0.001) and from 5% to 2% for PTB+ (X2trend, P,0.001). The treatment success was higher in rural areas (AOR 1.11; CI 95%: 1.03–1.2), less for PTB- (AOR 0.86; CI 95%: 0.80–0.92) and higher for extra-pulmonary TB (AOR 1.10; CI 95%: 1.02– 1.19) compared to PTB+. A higher lost-to-follow up was observed in men (AOR 1.15; CI 95%: 1.06–1.24) and among PTB- cases (AOR 1.14; CI 95%: 1.03–1.25). More deaths occurred in PTB-cases (AOR 1.65; 95% CI: 1.44–1.90) and among cases older than 65 years (AOR 3.86; CI 95%: 2.94–5.10). Lastly, retreatment cases had a higher mortality than new cases (6% vs 3%).
Conclusion: Over the past decade TB CNRs and treatment outcomes improved, whereas the disparities of disease burden by gender and place of residence reduced and mortality declined. Strategies should be devised to address higher risk groups for poor treatment outcomes.

